Empowerment, in its most basic sense, means giving people the tools, knowledge, and confidence to take control of their own lives. It’s not about someone else making all the decisions for you—it’s about having the voice, the choice, and the ability to shape your own path. Now, when we bring this concept into health and social care, it takes on an even more important role. Here, empowerment is about enabling individuals—patients, residents, service users—to take an active role in their own care and life decisions.
Why does this matter so much? Imagine being in a hospital or care home and feeling like every choice is made for you without your input. That feeling of helplessness can affect not just your mental health but also your recovery. Empowerment flips that script—it turns patients into partners rather than passive recipients of care.
Empowerment in health and social care is linked to improved recovery times, better treatment adherence, and higher satisfaction rates. It also aligns with respecting human dignity and rights, making care more personalised and compassionate.
This article will explore what empowerment in health and social care really means, why it’s essential, its benefits and drawbacks, strategies to make it happen, and real-life examples you can relate to. By the end, you’ll see why empowerment isn’t just a “nice idea” but a cornerstone of quality care.
Table of Contents
What is Empowerment in Health and Social Care?
Empowerment in health and social care refers to enabling individuals to have control over their care and life decisions, while providing them with the knowledge, skills, and support they need. It’s not simply about giving them information—it’s about ensuring they can understand, use, and apply it in ways that matter to them.

Here’s the difference: providing care means you do things for someone; empowering them means you do things with them. For example, a nurse might administer medication on schedule without discussion—that’s care. But if the nurse explains the medication’s purpose, potential side effects, and lets the patient decide the best time to take it within safe limits—that’s empowerment.
This concept is closely tied to patient rights, dignity, and self-determination. It’s about respecting that individuals are experts in their own lives. Even in situations where they may lack medical expertise, they still have valuable insight into their preferences, goals, and boundaries.
In health and social care settings, empowerment can take many forms:
- Giving patients access to their medical records.
- Involving them in care planning meetings.
- Allowing them to choose their meals, activities, or daily routines.
- Supporting them in learning new skills for independent living.
In short, empowerment transforms care from a one-way delivery into a two-way partnership.
Read Our Popular Blog: What is Health and Social Care? – A complete guide
Why is Empowerment Important in Health and Social Care?
Empowerment plays a critical role in improving not only health outcomes but also overall quality of life. Here’s why:
1. Improves Quality of Life
When people are empowered, they can make choices that reflect their values, beliefs, and preferences. This creates a sense of ownership and satisfaction. For example, allowing an elderly resident to choose their wake-up time rather than following a strict schedule can make them feel respected and valued.
2. Encourages Self-Advocacy
Empowerment equips people to speak up about their needs and rights. In healthcare, this could mean asking for a second opinion or questioning a treatment plan. In social care, it might involve requesting adjustments to living arrangements to suit personal needs.
3. Builds Trust Between Care Providers and Individuals
When providers actively involve individuals in decision-making, it creates transparency. People are more likely to trust and cooperate when they feel heard and respected.
4. Supports Mental and Emotional Well-being
Feeling in control of one’s life is closely linked to reduced stress and anxiety. In fact, research has shown that patients who are involved in their care are more likely to experience faster recovery and better emotional resilience.
Without empowerment, care can become paternalistic, leaving individuals feeling like passengers rather than drivers of their own journey. With empowerment, the journey becomes a shared road trip—the care provider might navigate, but the individual is in the driver’s seat.
Empowerment in Health and Social Care vs. Healthcare
While “healthcare” and “health and social care” are often mentioned together, there’s a subtle but important difference when it comes to empowerment.
Healthcare empowerment generally focuses on the medical aspects—patients being informed about diagnoses, treatment options, and prevention strategies. It’s about encouraging people to manage their own health and work collaboratively with healthcare professionals.

Health and social care empowerment, however, goes beyond the medical side. It includes social, emotional, and community aspects—helping individuals participate in society, maintain independence, and make decisions about their day-to-day lives.
For instance:
- In healthcare, empowerment might involve teaching a patient how to manage diabetes through diet and exercise.
- In social care, empowerment could mean helping that same person join a community cooking class so they can maintain social connections while eating healthily.
Community-based settings often take a holistic approach, focusing on well-being in all aspects, while medical settings may focus more narrowly on physical health. Both are important, but they require slightly different empowerment strategies.
Read Our Popular Blog: Effective communication in health and social care.
Pros and Cons of Empowerment in Health and Social Care
Empowerment in health and social care is a powerful approach that can transform the way individuals experience treatment and support. By giving people more control over their choices, it fosters independence and a stronger sense of dignity. However, just like any other practice, it comes with both strengths and challenges that need to be carefully managed for the best results.
Advantages
Empowerment in health and social care brings numerous benefits:
- Better Health Outcomes: People who understand and participate in their care tend to follow treatment plans more consistently.
- Stronger Relationships: Involving individuals in decisions builds mutual respect and trust.
- Increased Confidence and Independence: Over time, empowerment can lead to greater self-reliance, reducing dependence on services.

Potential Challenges
However, empowerment isn’t without its challenges:
- Risk of Wrong Decisions: Without proper information, individuals might make choices that harm their health.
- Delays in Urgent Care: Overemphasis on autonomy can slow down urgent interventions if too much time is spent on discussion.
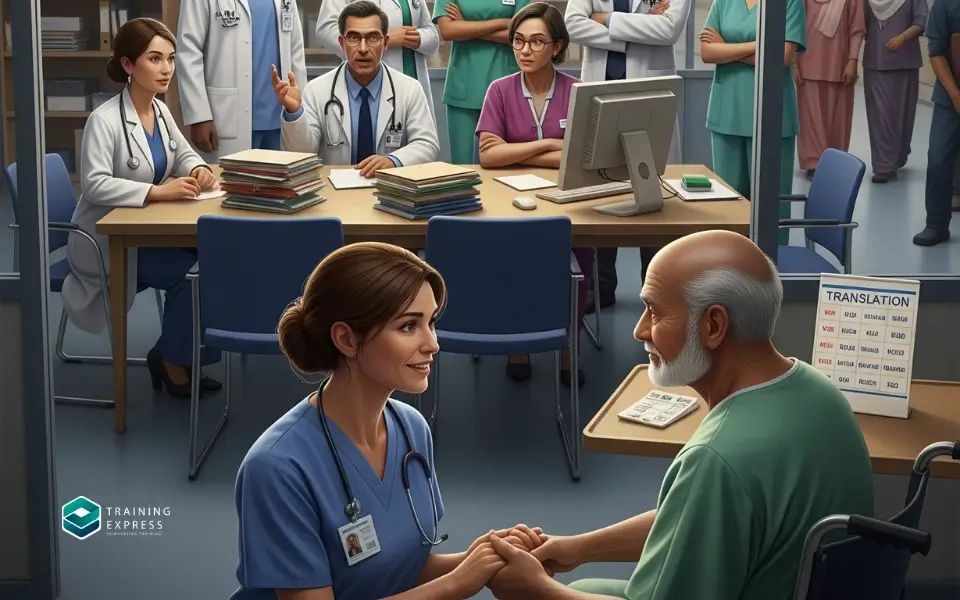
- Communication Barriers: Language differences, cognitive impairments, or lack of health literacy can limit effective empowerment.
Balancing empowerment with safety and practicality is key—it’s about guiding, not controlling, and ensuring individuals have the right tools to make informed decisions.
Factors Affecting Empowerment in Health and Social Care
Empowerment doesn’t happen automatically—it’s influenced by several factors that can either strengthen or weaken it. Understanding these elements is essential for care providers who want to make empowerment a real and sustainable practice.
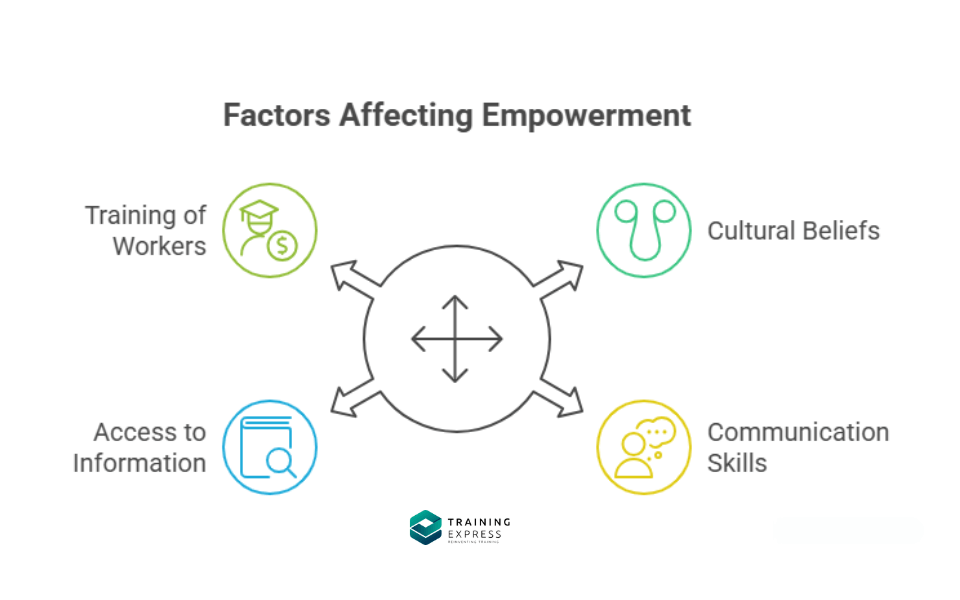
1. Cultural Beliefs and Values
Culture shapes how individuals perceive health, illness, and care. For example, in some cultures, family members traditionally make medical decisions rather than the individual. In others, speaking directly to a healthcare professional is encouraged. Being aware of these cultural differences helps providers respect beliefs while still promoting autonomy.
2. Communication Skills of Both Care Providers and Individuals
Empowerment is built on effective communication. A care provider may have the best intentions, but if they use complex jargon that the person doesn’t understand, empowerment fails. Likewise, individuals need the confidence and ability to express their needs clearly. Training in plain-language communication can bridge this gap.
3. Access to Information
Empowerment is impossible without accurate, timely, and understandable information. This means not just handing over leaflets but also ensuring that the person truly understands their options. Digital platforms, patient portals, and visual aids can make information more accessible.
4. Training of Health and Social Care Workers
Staff who are trained to listen, collaborate, and adapt their approach to individual preferences are better equipped to foster empowerment. Continuous professional development is essential to keep up with best practices.
Ultimately, these factors work together. If cultural sensitivity, good communication, and information access are in place, empowerment becomes far more achievable.
Read Our Latest Blog: Key Roles and Responsibilities in Health and Social Care Settings.
Empowerment Strategies in Health and Social Care
Empowerment isn’t a one-size-fits-all process—it requires tailored strategies depending on the setting and the individual’s needs. Here’s how it can be applied in different areas:

General Strategies
- Shared Decision-Making: Involve the individual in discussions about treatment or care plans. Present all options, explain risks and benefits, and listen to their preferences.
- Patient Education and Awareness: Knowledge is power—providing educational resources builds confidence and independence.
- Active Listening and Respect for Preferences: Acknowledge and validate what the person says, even if you can’t always meet their request exactly.
Empowerment in Aged Care
- Respecting Choices in Daily Routines: Allowing residents to choose meal times, bathing schedules, or clothing can significantly improve their sense of control.
- Encouraging Community Participation: Organising group activities and outings keeps individuals socially engaged and mentally stimulated.
Empowerment in a Care Home
- Involving Residents in Care Planning: Residents should be part of discussions about their treatment and lifestyle arrangements.
- Promoting Social Engagement: Activities like book clubs, exercise groups, or gardening projects encourage community involvement.
Empowerment in Home Care
- Supporting Independence in Personal Care: Assist without taking over—allow individuals to do what they can for themselves.
- Allowing Flexibility in Care Routines: Adapt care schedules to the individual’s preferred lifestyle whenever possible.
By applying these strategies, health and social care providers can move away from a “service delivery” mindset and toward a partnership model where the individual’s voice is at the center of decision-making.
Promoting Empowerment in Health and Social Care

Promoting empowerment is more than just a set of strategies—it’s a mindset shift across the whole system.
1. Role of Training and Continuous Education
Staff should be trained in communication, cultural competence, and person-centered care. Ongoing learning keeps them updated on best practices and new tools for empowerment.
2. Use of Technology and Communication Aids
Digital health tools such as apps, telehealth services, and patient portals give individuals more control over their health information. Communication aids like picture boards or translation apps can help overcome language and literacy barriers.
3. Policy Support and Organisational Culture
Empowerment thrives in an environment where policies actively support patient rights and participation. This requires leadership commitment to a culture that values collaboration over control.
A healthcare setting where empowerment is prioritised will often see better outcomes, higher satisfaction rates, and more engaged patients and residents.
Key Issues and Barriers to Empowerment in Health and Social Care
Even with the best intentions, empowerment faces real-world obstacles.
1. Lack of Resources and Staff Shortages
Overworked staff may not have the time to fully involve individuals in decisions. Empowerment requires patience, and that can be hard to achieve in understaffed settings.
2. Inconsistent Communication
Mixed messages from different professionals can confuse individuals and undermine trust. A unified approach is essential.
3. Discrimination or Bias
Prejudice—whether based on age, gender, race, disability, or other factors—can limit opportunities for empowerment. Providers must actively work to counteract bias.
4. Resistance to Change
Some professionals may feel that involving patients in decision-making undermines their authority. Likewise, some individuals may be hesitant to take on more responsibility for their care.
Addressing these barriers means making systemic changes and challenging outdated attitudes.
Risks of Empowerment in Health and Social Care
While empowerment is generally a positive approach, it’s important to acknowledge that it’s not without its risks. If not handled carefully, it can lead to unintended consequences that affect both the individual and the care provider.

1. Possibility of Unsafe Choices
When individuals are given full autonomy, there’s always the chance they might make decisions that compromise their health or safety. For example, a patient with a serious infection might refuse antibiotics due to personal beliefs, potentially worsening their condition. While respecting autonomy is vital, care providers must balance it with their duty to protect well-being.
2. Conflicts Between Autonomy and Medical Advice
Sometimes, a person’s choices may directly conflict with professional recommendations. A patient might want to stop taking essential medication because of side effects, while the doctor insists it’s necessary. These situations require careful negotiation and clear communication to avoid confrontation.
3. Emotional Strain on Individuals When Facing Complex Decisions
Not everyone wants to take full responsibility for their care decisions—some people find it stressful or overwhelming. This is especially true in cases involving serious illness or end-of-life care, where choices are emotionally charged. Empowerment should never mean forcing responsibility onto someone who isn’t ready for it.
To manage these risks, providers need to ensure that empowerment comes with support, education, and guidance, so that autonomy is exercised safely and confidently.
Examples of Empowerment in Health and Social Care
Understanding empowerment is easier when you can see it in action. Here are some real-life examples that show how it works in different settings:

Case Study – Involving a Patient in Treatment Planning
Maria, a 45-year-old with chronic arthritis, was frustrated by constant medication changes. Her care team decided to hold a shared decision-making meeting, presenting all available treatment options, side effects, and likely outcomes. Maria chose a combination of physiotherapy and a lower dose of medication, which worked better for her lifestyle. This gave her control while still ensuring safe, effective treatment.
Everyday Examples:
- Meal Choices: In a care home, residents are given menus and allowed to select meals based on their preferences and dietary needs.
- Mobility Aids: A patient recovering from surgery chooses between different types of walking aids after being shown how each works.
- Activity Participation: A social care worker invites residents to suggest activities for the monthly calendar, giving them a voice in community life.
These examples show that empowerment doesn’t always require grand gestures—it can be as simple as offering options and listening.
Final Thoughts
Empowerment in health and social care is far more than a trendy concept—it’s a fundamental shift in how care is delivered. It puts individuals at the heart of decision-making, respects their dignity, and acknowledges their expertise in their own lives. While there are challenges and risks, the benefits far outweigh them when empowerment is done thoughtfully and collaboratively.
From improving quality of life to fostering trust and independence, empowerment changes the dynamic from “care provider and passive patient” to partners in care. The key is to ensure that autonomy is supported by the right information, resources, and guidance.
As the health and social care sector continues to evolve, adopting empowerment-focused practices will be crucial for achieving better outcomes and building stronger, more respectful relationships between providers and those they serve.
Frequently Asked Questions (FAQ)
What do you mean by empowerment?
Empowerment means giving individuals the knowledge, confidence, and resources to take control of their own decisions and actions.
What is an example of empowerment in care?
Allowing a patient to choose their treatment plan after understanding the options is a clear example of empowerment.
Who defines empowerment?
Empowerment is defined both by professional guidelines and by the individuals themselves, as it’s about personal choice and autonomy.
What is empowerment and give an example?
Empowerment is enabling someone to have control over their decisions—for example, a resident choosing their daily routine in a care home.
What are the barriers to empowerment in health and social care?
Barriers include lack of resources, poor communication, cultural misunderstandings, and staff resistance to change.
What are the current issues in health and social care?
Key issues include staff shortages, funding challenges, and the need for more person-centered approaches.
What are the risks of empowerment in health and social care?
Risks include unsafe choices, conflicts with medical advice, and emotional stress from decision-making.
Why is empowerment important in healthcare?
It improves treatment adherence, builds trust, and enhances patient satisfaction.
Why is empowerment important in social work?
It helps individuals regain control over their lives, boosting confidence and independence.
How can empowerment be promoted in care settings?
Through education, shared decision-making, effective communication, and respect for personal preferences.
Related Blogs
- Available Courses
- Animal care10
- Design28
- Training9
- Accounting & Finance Primary49
- Teaching & Academics Primary37
- Teaching23
- Quality Licence Scheme Endorsed175
- Law10
- IT & Software229
- Job Ready Programme52
- Charity & Non-Profit Courses28
- HR & Leadership4
- Administration & Office Skills4
- Mandatory Training36
- Regulated Courses4
- AI & Data Literacy24
- Health and Social Care290
- Personal Development1623
- Food Hygiene119
- Safeguarding80
- Employability288
- First Aid73
- Business Skills294
- Management425
- Child Psychology40
- Health and Safety532
- Hospitality28
- Electronics31
- Construction62
- Career Bundles201
- Marketing39
- Healthcare172

 Food Hygiene
Food Hygiene Health & Safety
Health & Safety Safeguarding
Safeguarding First Aid
First Aid Business Skills
Business Skills Personal Development
Personal Development